Ethiopia has a long history of hosting people fleeing war and persecution.
The country’s current refugee policy, in place since January 2019, is one of the most progressive in Africa, if not the world. Since conflict broke out in neighbouring South Sudan in late 2013, Ethiopia has welcomed more than 900,000 refugees who have crossed the border in search of safety. Almost half have settled in Gambela, a rural region with a punishing climate which lies to the west of the country. In fact, Gambela’s population has almost doubled since the fighting began.
This rapid growth means additional stress has been placed on an already-stretched health workforce: Gambela is under-resourced in almost all areas, and there is a critical shortage of lab technicians, pharmacists, and midwives. According to the 2018 Human Development Report, only 27.7% of births in Ethiopia are attended by a skilled health professional*. But a new generation of health workers is setting out to change things for the better – with support from the NGO Amref Health Africa.
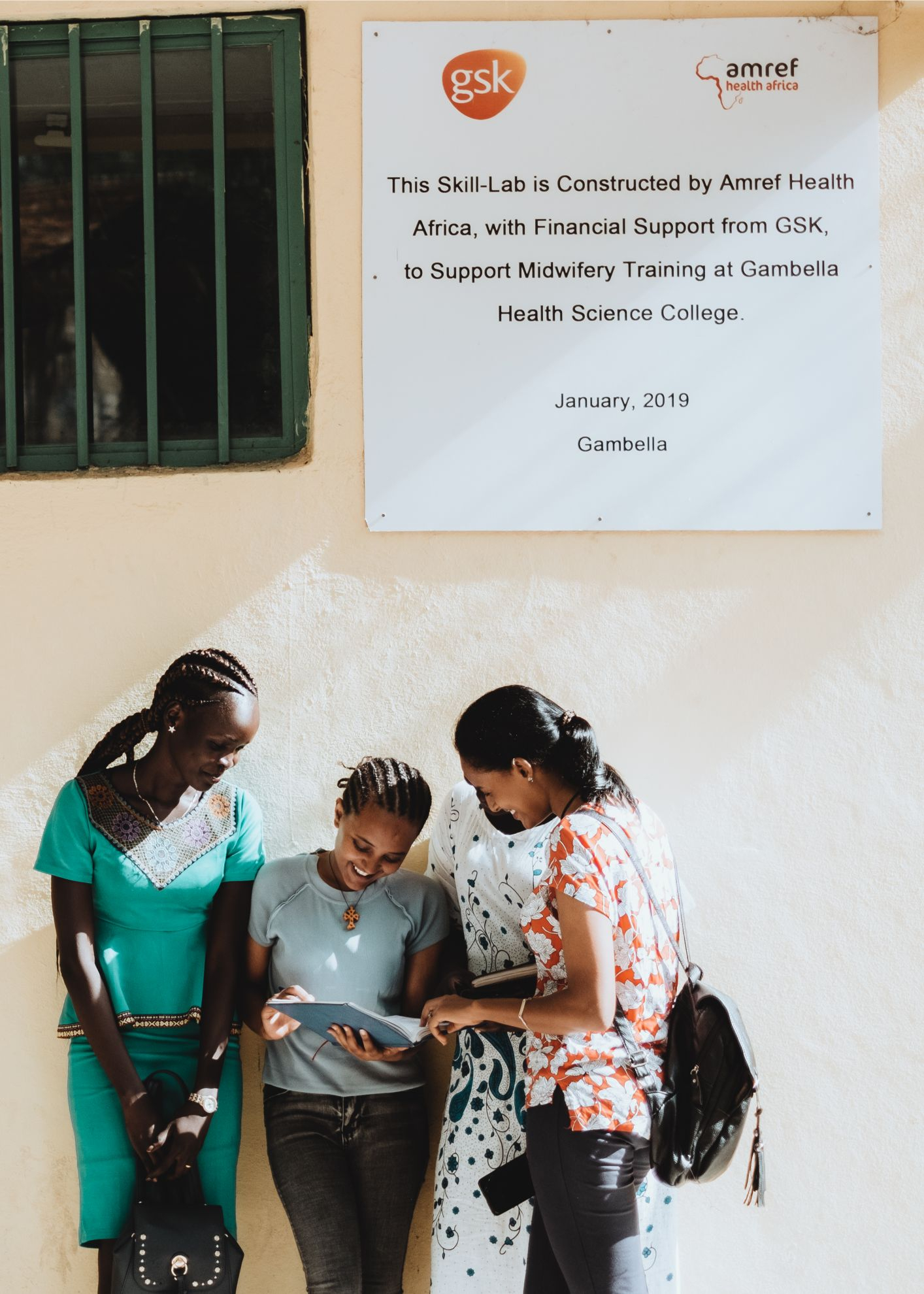
© Girma Berta for Amref Health Africa
Building skills to fill a gap
“Health worker training is one of the pillars of Amref Health Africa’s work in Ethiopia, and this includes Gambela, where the need is very acute,” says Project Officer Woinshet Tesfaye. “We are working to increase the number of health workers operating in the region, and to improve the quality of services they deliver to the people who live here.” Amref has supported the establishment of a midwifery training programme at Gambela’s Health Science College. The three-year course is a combination of classroom sessions, practical demonstrations, and hospital placements. to date, 67 midwives have graduated and been deployed throughout the country. By May 2020, 190 midwives will be enrolled in the programme in Gambela – all of them young women.
“Previously, there was no midwifery training available in Gambela, and students had to travel hundreds of kilometres if they wanted to follow this career path,” explains Woinshet. “This meant that a lot of very capable, passionate candidates were excluded. And the drop-out rate was very high.”

© Girma Berta for Amref Health Africa

© Girma Berta for Amref Health Africa
We became midwives to save our community.
Infant mortality rates in Gambela are higher than the national average. The majority of women here give birth at home. This is due partly to the shortage of midwives at health facilities, and partly to traditional beliefs and practices surrounding pregnancy and birth.
“As part of our course, we learn how to protect the dignity of our patients, how to respect them,” says second-year student Nyabuay Chuol (pictured at top). “We also learn about cultural matters: there are a lot of different ethnic groups here in Gambela. We learn about different beliefs and practices, and how to accommodate them.”
Ayachuol Lual, another second-year student (pictured below), nods enthusiastically. “When we are health workers, we can give health education in the communities. So, we will advocate in the community and encourage women to come to health centres. We became midwives to save our community, to save mothers and their new-borns.”

Be strong, be confident, and love your job.
Ayachuol’s journey to becoming a midwife started with a chance encounter a couple of years ago. “It was like a dream,” she remembers. “As I was just walking on the roadside I saw a woman giving birth: traditionally, with no-one to help her. I was scared. We all [passers-by] tried to assist her by taking her home, but there was still no medication to give her. Since I came to school I’ve learned that when mothers give birth, when there is excessive bleeding, there are medications you can give. But during that time there was none. But she survived, and the baby survived. I stayed with her as she was giving birth. And I still visit her at home today! She is one of my near neighbours.
“That day, something came into my mind. I said to myself, I wish I would be a midwife one day.”
So what advice would she give to someone who’s considering following the same path? She answers immediately. “I would tell them to be strong, be confident, and love your job.”

* In Uganda, the equivalent figure is 74.2% – and this indicator isn’t even recorded for the UK. Source: 2018 Human Development Report: http://hdr.undp.org/en/countries/profiles/ETH.
_______________________________________________________________________________________________
Amref Health Africa partners with women and girls in more than 30 countries to improve access to healthcare and break the cycle of poverty. Amref UK’s current campaign, Health in Her Hands, celebrates and supports the frontline health workers who are saving and changing lives across Africa.
Until 7th June, all public donations to Health in Her Hands will be doubled by the UK government. To find out more, visit the Amref UK website or find them on social media @Amref_UK.