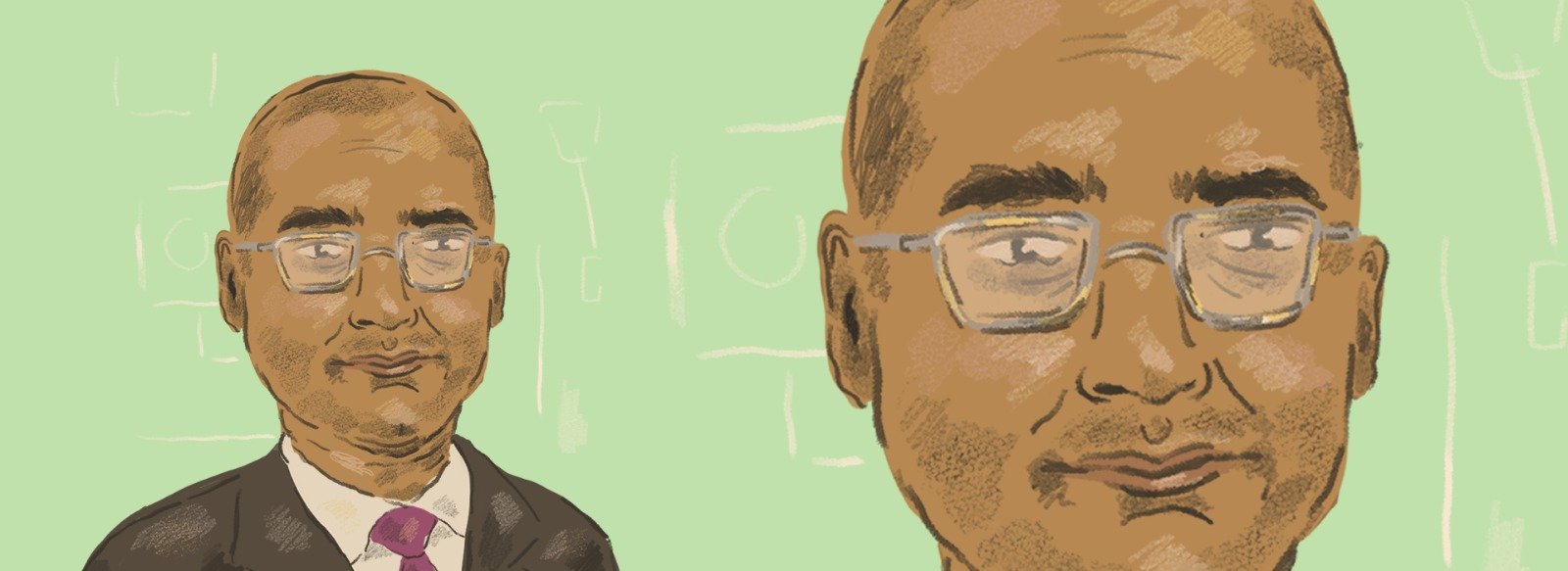
With a lot of media attention focused on hospitals and the amazing work that doctors and nurses are doing within them, shado sat down with a London GP to discuss how his practice has been dealing with COVID-19 and the potential positive effect that this pandemic might have on NHS operations.
Unlike most members of the UK public, for whom coronavirus was a distant reality long before it majorly affected their lives, Michael* was forced to completely restructure his clinic overnight upon the announcement of lockdown measures. This manifested in the form of a ‘triage’ model, which he explains meant: “no face to face consultations and no one coming into the building unless they had been assessed by a doctor or a nurse and deemed ‘need to be seen’.” This model was managed online with patients filling out proformas and doctors then deciding whether a telephone or video call, or in extreme cases, a face to face consultation, was necessary. Of the new system he says: “it’s been quite phenomenal really [the change] from what we were doing to what we’re doing now”.
I ask him whether this was a smooth transition and he chuckles slightly, “Has it been smooth?” he repeats. “Necessity has demanded it”. He goes on to explain: “had we done it outside of a pandemic, it would have taken months, if not years, of planning and what ifs.” As it stands, the change was completed in just four days, an incredible feat which was replicated in clinics across the country. “I think that everyone realised that if we wanted to keep patients and staff safe we’d have to do things very differently and that’s why it fell into place so quickly.”
One of the biggest challenges of this new system seems to be the amount of patients who are now avoiding the clinic all together. Scared of mixing with the public and unaware of the online system, people are now starting to experience long-term health concerns as conditions and diseases which could have been managed much more easily if caught early, have now progressed. For example, Michael states that in some cases those who have suffered from a stroke “who would normally be able to get that treated quite quickly, are now left with the disability of that stroke”. Sadly, Michael has noticed that even parents with young children have been hesitant to attend in some cases. “COVID-19 isn’t as high of a cause of illness in young children, so when they’re sick there’s probably something else going on”.
Michael also faces complexities with the patients that do contact the clinic with non COVID-19 related issues as they are often unable to treat them as effectively as they would wish. In the early stages, all our other usual services were ‘switched off’, so things like doing blood tests, X-rays, referring people to hospitals, all those routine services became restricted . So it’s been a problem when you’re dealing with someone who’s sick who needs something but you’re not able to get to the service you need to sort them out.”
Furthermore, unlike some of the expectations concerning the treatment of them, health issues that present alongside COVID-19 are unlikely to materialise instantaneously. The full financial and economic impact of lockdown is as of yet unknown but Michael points towards one area where the impact is certain: the community’s mental health. Again he outlines the risk for young people, highlighting the impact “of them not being able to go to schools and being cooped up all day” and the increased risk of harm from other causes. He further states: “That’s not just a virus epidemic, but that’s another type of epidemic that’s starting to emerge.”
It’s not only GP surgeries which were required to undertake a drastic transformation. Pharmacies, another essential community care body which has largely escaped media attention, faced, and continue to face, immense challenges due to lockdown. Michael states: “I think the community pharmacy sector has had a really tough time.” Like many NHS workers, pharmacists had issues obtaining PPE, however unlike surgeries, pharmacies stayed open, meaning they were dealing with a large volume of people face to face. Pharmacists were also not explicitly included in the key workers list which meant it was more difficult for them to access benefits such as special supermarket opening times and childcare, that were available to other NHS workers. Michael states that the best way to combat this is to raise awareness of all those working to battle coronavirus. “There’s clearly a lot of focus on doctors and nurses in hospitals and rightly so, but there are also a lot of people across multiple health and social care fields, as well as and all the utilities, that don’t always get a look in, who are working really hard to keep the show on the road.”
While plans for resuming ‘normal services’ are starting to come into effect with Matt Hancock announcing the reopening of hospital services last week, Michael hopes that a reopening won’t mean a complete reversion. “We want to retain as much of what we’ve been doing over the past few weeks as possible. Especially the ways in which we’ve managed demand and how we’ve coped with working together better. We don’t want to revert back to everyone fighting for an appointment!” Michael hints at a feeling of consensus in the medical community concerning this issue, explaining that many people believe the days are numbered for “hospital services which normally depend on someone driving to a hospital, spending a lot of money in the car park and then having a three hour wait before seeing a specialist for two minutes.”
He explains that this move towards a more technology friendly NHS had already begun prior to the outbreak, with consultant colleagues and nurses conducting remote consultations, “so there’s no reason why that can’t be done in a sustained way.” He also outlines the further potential benefits of this, including the positive environmental impact and how it will facilitate better communications between multiple NHS departments. The potentiality of technology to streamline certain NHS processes does indeed seem huge and allows, as Michael states: “a greater focus on the people who are ill … improving the way people are treated going forward.”
Recently there has been some concern surrounding the government using the crisis to sell off parts of the NHS to private companies, outsourcing PPE management to companies like Deloitte. Michael explains that this turn towards technology doesn’t have to mean an increase in privatisation however. Currently, as he points out, “there’s quite a lot of private services that operate within existing NHS structures. If you just think about all the tech, medicines, diagnostics, the particular types of treatment, the monitors etc. So, while there may be contracts with private companies, I think the key question is do we maintain a service that is free at the point of use and is accessible by all? And personally, I can’t see that changing.”
Rather, Michael states, technology could possibly be used to encourage NHS processes to become more effective, which could potentially take away the need for private interference. At the very least the increase in tech usage has encouraged the different departments in the NHS to work together. Which as Michael points out, hasn’t always been the case. “Sometimes within the NHS there have been rivalries created, hospitals and GPs, GPs and Pharmacists, Doctors and Nurses, you get the picture. I’m really hoping that this has shown us how we can collaborate more around the things that matter to us: our patients. I know that sounds a bit trite but I genuinely feel that there’s been a spirit of ‘we can all get on this together if we work together’, so I’m hoping that culture continues and maybe can be enhanced.” Michael also hopes that this feeling of working together can be reflected in the funding different areas receive as he explains that traditionally the majority of NHS funding goes to hospital care. “I’m hoping that as a result of this people will be interested in the value of community care. By this I mean not just general practices but pharmacies, community services, mental health services and social care. It would be really good to see significant investment in the areas which matter most to people and communities. A literal turn of the dial towards community services would be great.”
While this pandemic has pushed our health services to extreme lengths, it has also created a climate of efficacy which has allowed the modernisation of practices. It has also enabled different branches of the NHS to work together more easily, allowing them to better continue the incredible work they accomplish, and are often not adequately recognised for. As Michael states: “Great teams are made, not by individual players, but by how they work together for a common purpose.”
*Name changed to protect identity.