A few days before I spoke to doctor, activist and writer Annabel Sowemimo, my mother was unexpectedly admitted to hospital, needing semi-urgent treatment. Warm and soft, her perma-smile belies a matriarchal fierceness that had raised five younger siblings, traversed continents over land and sea fleeing war, and started life afresh thrice. Yet these details were shed with her clothes. The hospital gown that replaced them left little more than what met the clinical eye: a brown, barely-five foot, sixty-something, with second-language English and a ‘strong family history of heart disease.’
Despite its popular claims of universality, the NHS has never truly been a place of care and safety for all. Instead, it has been a site of structural violence that – just like many of our contemporary public institutions – socially reproduces hierarchies of power. These hierarchies position those racialised as Black and brown, particularly from the working class, at the sharpest edge of harm from these systems, culminating, as Ruth Wilson-Gilmore puts it plainly, in “premature death.”
As a doctor within the NHS, I have been very proximate to this violence, towards both patients and workers. But the embodied experience of navigating this as a relative was clarifying. Mum, through me, had layers of protective social capital – my working knowledge of the system, favours from networks of colleagues to sense-check decisions and friends working at the hospital that could make her time there slightly less isolating. And yet, her experience was one of near misses, of not being listened to, of being made to feel small.
It was amidst this that I landed at the door of Annabel’s book, Divided.
From Decolonising Contraception to ‘Divided’
As Annabel and I discuss, although we’ve ‘grazed’ past each other in different spaces and our ecosystems overlap, we’ve never actually spoken to one another before this. What is clear from our conversation, her writing and her broader legacy of work, is that Annabel comes with an alchemic mixture of lucid communication, emotional vulnerability and deep academic rigour.
Of course, this makes sense – she is a transdisciplinarian. While working as a clinician (a registrar in community sexual and reproductive health in Leicester), researcher (completing her PhD), writing and broadcasting widely, she is also involved in community organising and engagement through the Reproductive Justice Initiative (formerly known as Decolonising Contraception), which she co-founded.
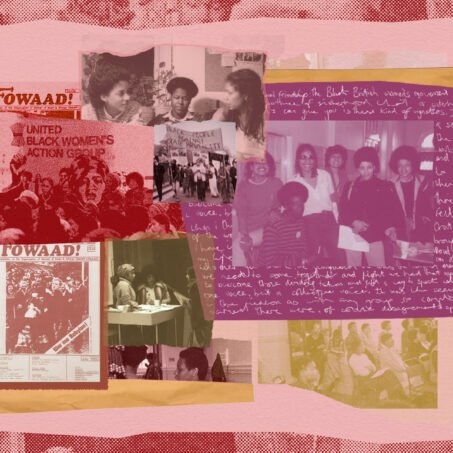
It is in the context of Decolonising Contraception that I first came across Annabel. The group is a “collective of sex educators, clinicians, campaigners, journalists, researchers, and community organisers,” starting out as a place for people of colour to have discussions that weren’t being had in the mainstream around sex, relationships and reproductive health.
In the same year that Decolonising Contraception was founded, Annabel started writing a regular feature for gal-dem (a media outlet that recently and heart-breakingly disbanded), called Decolonising Healthcare. It is this that ultimately evolved into the book.

Race, colonialism and health inequities
While the importance of health inequities along lines of race has finally started to be recognised over the last few years, most published research and policy-related literature within the UK stops short of naming racism – structural or otherwise – as a determinant of poor health.
In the context of a government that denies the existence of institutional racism, the political and legislative landscape in the UK has become markedly more hostile towards racialised people and their health.
Racialised health inequities in the UK are stark by any measure, qualitative or quantitative, across almost all modalities of health. But meaningful action has been lacking. Despite media coverage over several years and a dedicated government taskforce, the chasm in standards and outcomes of maternal healthcare for Black women remains unchanged.
Mental health care is no better. Black children are 10 times more likely to access mental health care through social services (rather than GPs) compared to their white counterparts. In a similar vein, Black and minority ethnic adults are 40% more likely to access mental health services via the criminal justice system than white people.
The NHS Race & Health Observatory was launched in 2020 as an independent body to “identify and tackle the specific health challenges facing people from BAME backgrounds.” Yet it has failed to move beyond the problem diagnosis phase, compiling evidence and putting forward recommendations, with no ostensible translation into policy or practice.
Racialised folk are overrepresented within the health and care workforce, and racism is similarly rife. Racialised staff are disproportionately exposed to occupational risks as seen during the pandemic. The race pay gap continues to be significant. And the casual precarious employment – especially of migrant workers – remains common. However, conversations within the NHS are stuck discussing the merits of representation and diversity in leadership, unable to coalesce a meaningful structural analysis or formulate what may need to change.
And yet amongst all of this, as Annabel sets out, accessible scholarship around the colonial fingerprints on present-day racialised health inequities has been almost completely absent from the UK discussion.
In this vein, one of my first questions was about who the book was for.
As several of the book endorsements set out, the text is a must-read for healthcare practitioners. However, to enclose this as the most relevant audience for this book does it a disservice. As we catch up, Annabel explains that it was intentional to not go with an academic publisher. “I don’t feel like there’s been anything that’s trying to be mainstream in terms of trying to appeal to the needs of different readerships,” she explains – and this is the gap she wants to bridge.
Ultimately, Divided is for a popular audience, and it is in this context that the book should be understood. This is reflected in its ‘methodology’ and voice: Annabel weaves archival research, policy analysis and interviews with key figures across activism, clinical practice and academia. But the chapters are also coated with personal stories that season the prose, providing a vulnerability that feels not just like a rhetorical tool, but an authentic and important regrounding of her own experiences navigating these realities. She shares stories from her childhood, hurdles at medical school and most poignantly her experience of her late grandma’s hospital admission with a stroke.
Annabel’s personal motivation and relationship to the content of the book is evident – a product of her own reckoning as a Black clinician and woman genealogically “intertwined with the NHS” and its story. As Annabel shares in the book, her father is a doctor who trained in Ibadan, Nigeria at an outpost of University College London (Annabel’s own medical school), while her mother also had a period of service in the NHS. And as she sets out at the end of the book, her beloved grandmother was an auxiliary nurse at the Royal Free Hospital from the early 1960s.
Decolonising healthcare?
Annabel’s location of herself within the story is explicit, and it brings our conversation to the topic of decolonisation within the book. She acknowledges the challenges of positioning herself as writing from a decolonial perspective on this topic, and notes that there were times she was unsure whether this was a story she should be telling.

Join our mailing list
Sign up for shado's picks of the week! Dropping in your inbox every Friday, we share news from inside shado + out, plus job listings, event recommendations and actions ✊
Sign up for shado's picks of the week! Dropping in your inbox every Friday, we share news from inside shado + out, plus job listings, event recommendations and actions ✊
“I am this person of mixed backgrounds in the global North. Will people question whether I’m the right person to try to bring decolonisation in this way into the mainstream?”
The current discourse around decolonisation and health is textured, but comes to the fore largely in relation to ‘global health.’ In many ways, the decolonisation of global health and its institutions is oxymoronic, particularly its tendency to overlook the materiality of reparations, landback and a reconfiguration of the entire matrices of power to create something unrecognisable to the present.
Snippets of the book hint towards this conversation. The chapter ‘Our Health Policy is Sick’ speaks, amongst other things, to the US global gag rule – where any NGOs receiving global health funding from the US government can’t provide legal abortion services – and on the outsized role of philanthrocapitalism. ‘Educating Differently’ mentions the need for expanding our views of what constitutes healthcare. Indeed, the book’s publishers, the Wellcome Collection, have been navigating their own relationship to these issues. Most recently, they closed their long-standing Medicine Man exhibition for “perpetuat[ing] a version of medical history that is based on racist, sexist and ableist theories and language,” replacing it with Grace Ndiritu’s The Healing Pavilion.
But this is not how the book is framed. Instead, Annabel pulls the concept of decolonising into meaningful dialogue with healthcare as a whole, rather than global health. I think this is a powerful and clarifying reframing that invites an examination and reconstruction of healthcare itself that is more expansive. In Annabel’s words, “decolonising healthcare means radically reimagining the structure of our society.”
The range of the book is astounding, cutting across topics and disciplines while maintaining coherence throughout. Annabel opens the book by providing a pithy, whistlestop tour of the direct colonial origins of race science, and how this continues to underwrite medicine today. The book goes on to traverse everything from clinical trials and perceptions of pain to health policy and technologic justice.
In her chapter ‘Carcerality is not the Cure’, Annabel does a brilliant job of introducing the relationship between health and the prison-industrial complex to someone that may be new to this linkage.
She traces a conceptual path from the race science-grounded beliefs that “Black people are inherently predisposed to crime.” This logic then follows that these people must be sequestered from society, whether through incarceration or the death penalty – something which is supported by the medical profession as an adequate therapeutic response. All the while, discussions – surrounding the conditions that may force certain decisions and the legal frameworks that criminalise these behaviours – are prevented. Annabel tells me she believes that “we have power to dismantle this [prison-industrial] complex that exists because we helped put it there.”

Epistemologies of healing
In the last few years, I have been wrestling with the violence of the Western biomedical paradigm on the one hand, and yearning to study and embrace other epistemologies of healing in my practice on the other. But through the chapter ‘Whitewashed,’ Annabel helps change my orientation, suggesting the distinction between these is a false dichotomy – and that the reality is in fact more complex and beautiful.
She shares the story of Onesimus, an enslaved man of Black African descent, who appeared immune to the deadly and rampant effects of smallpox following a local procedure that would be considered inoculation almost a century before Edward Jenner. As historian Londa Schiebinger sets out in her book, the exchange of knowledge between Europeans and those they colonised was ‘promiscuous and multi-directional’. This empirically disrupts white supremacist conceptualisations of colonisers from the metropole enlightening the ‘natives’. But more interestingly, it shows that to stringently silo so-called Western biomedical knowledges and Indigenous ones is fallacy – with loss of how these epistemologies conversed with one another.
To Annabel, this brings about a melancholy. “There’s a grieving process here,” she explains, “because when you look even now, lots of communities (as a result of these colonial processes) are far worse off and don’t have access to the resources they need. So many of us will never fully understand what our places were like or how our communities were before.”
The book focuses in several other places on education, and the conversation naturally pivots to the university and the question of knowledge production – Annabel is also a researcher after all. Acknowledging the richness of resistance and thought from certain scholars working within academic institutions, my provocation is whether the academy is capacious enough to hold radical futurity and reconcile these plural epistemologies of healing, particularly in the world of medical research.
For Annabel, while not an inclusive or welcoming place for racialised folk, particularly women, the academy represents “one of the only ways to produce what is considered valid, ethical, publishable research” which she says “is really frustrating.”
This is not without complications – in particular she cites the work of the late Dr Azeezat Johnson, who wrote on the exoticisation of “Black bodies” as fixed categories and spectacles in research conducted within the gaze of white academia.
Annabel also notes that for her, it is a matter of forging a path for racialised people, particularly Black women, and if at all possible making the alienating process of applying for positions and working in the academy “easier for the next person.”
I ask her, jokingly, whether the university will ever love us. Annabel laughs. “I think they love investigating us, that’s for sure; they love the spectacle of examining the ‘other,’ as long as we’re not examining ourselves,” she says.
Indeed, as she goes on to explain, academic discipline matters. She argues that it doesn’t go down well when “people come in and try to change up the narrative.” Crucially, the neoliberal university’s extractive, profit-centred strategies “guide what is taught, and who is employed, and who is seen as important.” Projects like the Free Black University give us hope that a different configuration is possible – but they remain islands in the sea of the academic-industrial complex.
La Coyuntura and the constellation
Let me return back to mum’s experience, and those of countless racialised folk who have had any contact with our dominant paradigm of Western biomedicine and the NHS. Of the many contributions of this book, perhaps the most poignant is the powerful analytic and historiographic body and language it provides communities of colour that are simultaneously gaslit while facing – in Engel’s words – the ‘social murder’.
We appear to be at a relative zenith of politicisation around the state of NHS. Its systematic under-resourcing is a form of organised state abandonment that disproportionately harms the health of working class, racialised folk, both workers and patients. Fundamentally, however, the state of the NHS is only one facet of the conversation around health for all.
The sustained health of the body politic depends on a deep interrogation and dismantling of our current configurations of state healthcare and its articulations with healing imaginaries that are already abundant by necessity at the community level. We must de-privatise the concentration of knowledge and power within the formal health system, and as Adler-Bolton sets out, close the gap between healthcare workers and patients – to organise together.
Coloniality has determined the contours of clinical practice in service of domination rather than care; to move beyond this surely demands a reparatory approach, as determined by those harmed? This line of thinking has started being explored specifically within a frame of transatlantic chattel slavery in the United States. What would it look like to reflect on this within the UK?
I often come back to the work of Aurora Levins Morales for guidance. She introduced me to this term – la coyuntura: “If the big picture is a constellation of stars by which we plot our course, the coyuntura is the muddy ground we stand in while we stargaze. The bloody, difficult present. Some of what we want to build can’t yet be done. Standing there in the mud, our job is to keep talking about stars while we shovel slush, add gravel, pass around hot thermoses. Sometimes that means supporting solutions that are painfully inadequate, that cost us, but still move us toward the universally humane future we long for.”
From my positionality as a healthcare worker, knotted into the state violence both as agent and recipient, standing in la coyuntura and reading Annabel’s book, I reflect deeply on what my role is, what our role is in this radical reimagining.
What does it mean to truly practise in service of collective self-determination for us all – patients, workers and beyond? In addition to large-scale visioning, that question includes an explicit invitation asking what abolitionist, radical healthcare looks like now.
What are the non-reformist reforms on that journey that we can facilitate, “the painfully inadequate” solutions as Levins Morales puts it? Is it upskilling and resourcing people in the community on basic suturing and wound care, such that a hospital admission and possible sectioning of a neighbour who has self-harmed in a mental health crisis can be avoided? Is it facilitating knowledge sharing around procurement and enabling testing of otherwise unaffordable, life-saving generic medicines sourced through buyers clubs?
Annabel’s book is an accessible and searing exposition of the coloniality of our current healthcare paradigm. Crucially, though, it is also a clarion call not just for healthcare professionals but for us as a body politic to see the “rotten foundations” of our understandings of health – and to organise collectively for decolonial, abolitionist futures.
What can you do?
Read:
- Divided by Annabel Sowemimo
- Health Communism: A Surplus Manifesto by Artie Vierkant and Beatrice Adler-Bolton
- Inflamed by Rupa Marya & Raj Patel
- Medicine Stories: Essays for Radicals by Aurora Levins Morales
Listen:
Watch:
Follow: